CPT 99494 Description, Billing Rules, & Use Cases
CPT 99494 is an add-on billing code used to report each additional 30-minute block of Collaborative Care Model (CoCM) services beyond the time covered under CPT 99492 or 99493.
It applies to non-face-to-face psychiatric care delivered by a behavioral health care manager, in collaboration with a psychiatric consultant and under the supervision of a billing provider.
This code can be billed alongside 99492 or 99493 when total CoCM time exceeds the base threshold—but may never be billed alone.
What is CPT Code 99494?
CPT 99494 is an incremental, time-based add-on code used within the Collaborative Care Model for behavioral health integration. It reflects continued patient engagement and care team coordination when total monthly CoCM time exceeds the limits of 99492 or 99493.
Use CPT 99494 when:
- You have already billed 99492 (initial month) or 99493 (subsequent months)
- Total collaborative care time reaches:
- 71+ minutes in the first month (99492 + 99494)
- 61+ minutes in ongoing months (99493 + 99494)
- The care team includes:
- A behavioral health care manager (BHCM)
- A psychiatric consultant
- A billing provider (physician, NP, or PA)
The code is used to report:
- Each additional 30-minute block of non-face-to-face team-based psychiatric care
- Services like case review, outcome tracking, care plan updates, and treatment coordination across the care team
CPT 99494 is only valid as an add-on to 99492 or 99493. Time must be clearly documented, and the patient must remain in an active CoCM care plan.
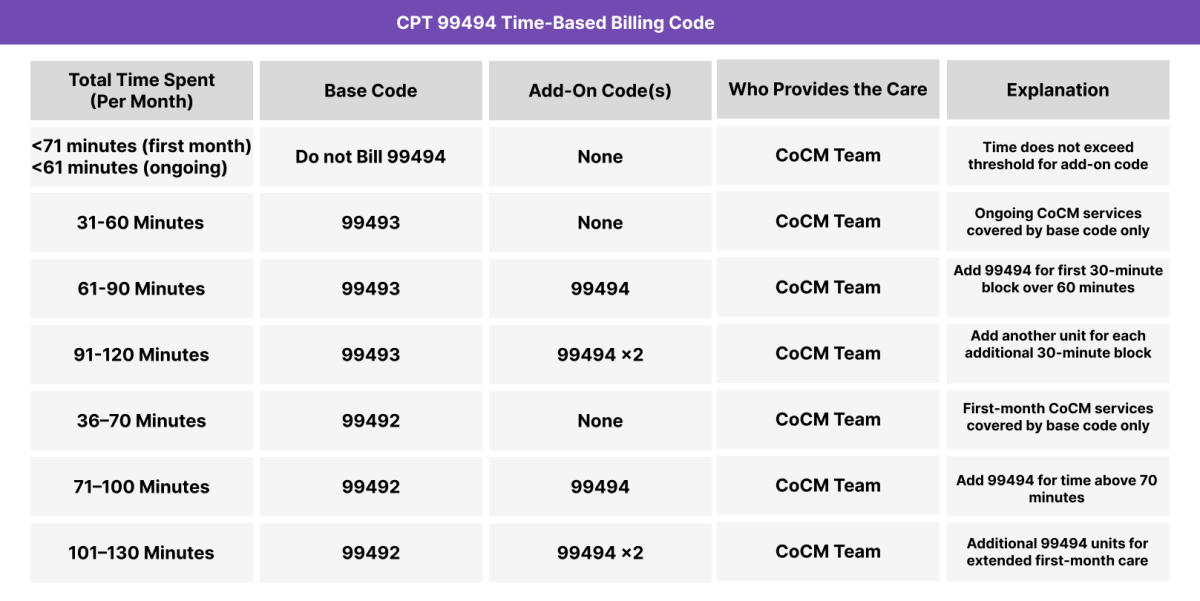
CPT 99484 Time Thresholds and Code Combinations
CPT 99494 is an add-on code used to report each additional 30-minute block of time spent delivering Collaborative Care Model (CoCM) services after the base time thresholds for CPT 99492 or 99493 have been met. This code reflects continued non-face-to-face psychiatric care coordination delivered by the CoCM team.
Important to Note:
CPT 99494 may only be billed with CPT 99492 or 99493 and never on its own.
It reflects each additional 30-minute block of CoCM time once:
- 70 minutes are exceeded in the first month, or
- 60 minutes are exceeded in ongoing months
All billed time must be:
- Non-face-to-face
- Logged with date, duration, and activity
- Performed by the full CoCM team under provider supervision
- Distinct from any other care management billing
When to Use CPT 99494: Common Scenarios and Use Cases
CPT 99494 should be used when total CoCM time exceeds the base thresholds covered by CPT 99492 (first month) or CPT 99493 (ongoing months). Each unit of 99494 accounts for one additional 30-minute block of time and reflects extended care team collaboration.
Here are examples of how CPT 99484 is used in practice:
CPT 99494 Billing Requirements and Eligibility
CPT 99494 is an add-on code used to report each additional 30-minute block of Collaborative Care Model (CoCM) services beyond the base time covered by CPT 99492 (first month) or CPT 99493 (subsequent months). It reflects ongoing behavioral health care coordination between a behavioral health care manager, a psychiatric consultant, and a billing provider.
To bill CPT 99494, the following requirements must be met:
Patient Eligibility Criteria
- The patient must have an active behavioral health diagnosis, such as:
- Major depressive disorder
- Generalized anxiety disorder
- PTSD or trauma-related disorder
- Substance use disorder
- The patient must already be enrolled in an active CoCM care plan
- The patient’s CoCM time has already reached the threshold for billing 99492 or 99493
Care Plan Requirements
- The CoCM care plan must be:
- Established in a prior month (under 99492)
- Updated or maintained in the current month
- Focused on measurable behavioral health outcomes
- Supported by validated assessment tools (e.g., PHQ-9, GAD-7)
- Shared and documented across the care team
Care Team Requirements
- The CoCM team must include:
- A billing provider (physician, NP, or PA)
- A behavioral health care manager (BHCM)
- A psychiatric consultant available for treatment input
- All roles must be documented by name and must collaborate on the patient’s care
Service and Time Requirements
- CPT 99494 may only be billed if total CoCM time exceeds:
- 70 minutes in the first month (with 99492)
- 60 minutes in any subsequent month (with 99493)
- Each unit of 99494 represents an additional 30-minute block
- All time must be:
- Non-face-to-face
- Delivered by the full CoCM team
- Accurately tracked and documented
Billing Limitations
- CPT 99494 may never be billed on its own
- It must always appear in conjunction with CPT 99492 or 99493
- Do not bill CPT 99494 in the same month as:
CPT 99494 Billing Documentation Checklist
CPT 99494 is a time-based add-on code and requires precise documentation of extended CoCM activity. To compliantly bill 99494, ensure the following are included in the patient’s medical record:
- A behavioral health diagnosis remains active and is the primary focus of care
- Example: MDD, GAD, PTSD, substance use disorder
- Diagnosis must be supported by ICD-10 and structured screening results (e.g., PHQ-9)
- A CoCM care plan is:
- Already in place (initiated under 99492)
- Maintained and updated during the billing month
- Shared across the team, with clearly documented clinical goals and interventions
- The full CoCM care team is active and documented:
- A base code (CPT 99492 or 99493) has been or will be billed in the same month
- CPT 99494 may not be billed independently
- Documented total time exceeds the base code threshold:
- More than 70 minutes total in the initial month (99492 + 99494)
- More than 60 minutes total in subsequent months (99493 + 99494)
- Time should be logged in a clear and auditable format (date, activity, duration)
- Activities performed during additional time must include:
- Outcome tracking or clinical assessment
- BHCM-patient follow-up
- Psychiatric case review and care plan revisions
- Interprofessional communication or coordination
- Provider attestation should confirm:
- Review of the care plan and BHCM documentation
- Active coordination with the psychiatric consultant
- Supervision of the CoCM process and continued care oversight
Common CPT 99494 Billing Mistakes (and How to Avoid Them)
❌ Billing 99494 Without a Base Code (99492 or 99493)
CPT 99494 may never be billed alone. It must appear on the same claim as either CPT 99492 (initial month) or 99493 (ongoing months). Billing it independently will result in rejection.
❌ Reporting Less Time Than Required
CPT 99494 requires total CoCM time to exceed:
- 70 minutes in the first month (with 99492)
- 60 minutes in subsequent months (with 99493)
If total time doesn’t cross the threshold, 99494 cannot be used — even if the month felt “busy.”
❌ Overlooking the Need for Team-Based Care
Time reported under 99494 must be collaborative and involve:
- A behavioral health care manager actively working with the patient
- A psychiatric consultant offering treatment input
- A billing provider overseeing and reviewing all care
Solo staff time or basic outreach doesn’t qualify.
❌ Stacking 99494 Without Matching Documentation
You can bill multiple units of 99494, but only if documentation supports:
- Total CoCM time
- Distinct 30-minute blocks
- Logged dates, durations, and descriptions of services
❌ Billing With Conflicting Care Management Codes
CPT 99494 cannot be billed in the same month as:
- 99484 (general BHI)
- 99490–99491 (Chronic Care Management)
- 99424–99427 (Principal Care Management)
- 99487–99489 (Complex CCM)
- 99495–99496 (TCM)
Each program is mutually exclusive. Only one set of care management codes may be billed per month per patient.



