CPT 99492 Description, Billing Rules, & Use Cases
CPT 99492 is used to bill for the first month of Collaborative Care Model (CoCM) services for patients receiving integrated behavioral health care.
This code covers the first 70 minutes of team-based psychiatric care delivered by a behavioral health care manager in coordination with a psychiatric consultant and the billing physician or qualified healthcare professional (QHP).
CPT 99492 may be billed only once per patient, and applies only to the initial calendar month of CoCM services. If time exceeds 70 minutes, CPT 99494 may be added to report each additional 30-minute block.
What is CPT Code 99492?
CPT 99492 is the introductory billing code for the Collaborative Care Model (CoCM) — a psychiatric care integration model that relies on structured coordination between a behavioral health care manager, a psychiatric consultant, and the patient’s primary care provider (PCP) or other billing QHP.
Use CPT 99492 when:
- The patient has a behavioral health condition such as:
- Major depressive disorder (MDD)
- Generalized anxiety disorder
- PTSD or other trauma-related conditions
- Substance use disorder
- A psychiatric consultant is engaged to provide treatment recommendations
- A behavioral health care manager works under general supervision to:
- Provide care coordination and brief interventions
- Track clinical outcomes using validated tools (e.g., PHQ-9, GAD-7)
- Facilitate communication between all members of the care team
- At least 36 minutes of CoCM activity is completed in the first calendar month
- Services are:
- Non-face-to-face
- Delivered by a coordinated team under the billing provider’s supervision
CPT 99492 may only be billed once per patient, and only for the initial CoCM month. Add CPT 99494 if total time exceeds 70 minutes. In later months, use CPT 99493.
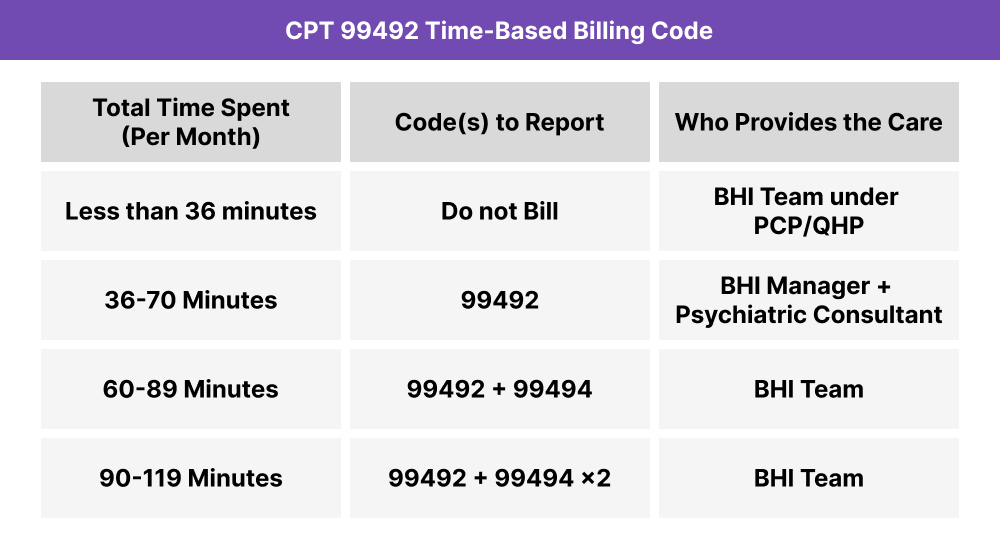
CPT 99492 Time Thresholds and Code Combinations
CPT 99492 is used to report the first 70 minutes of Collaborative Care Model (CoCM) services delivered in the initial calendar month of behavioral health integration. Services must be provided by a team of licensed professionals including a behavioral health care manager, a psychiatric consultant, and a billing physician or QHP.
Use the chart below to determine how to report time spent:
Important to Note:
CPT 99492 may be billed only once per patient, and only during the first month of CoCM services. If CoCM continues in subsequent months, use CPT 99493.
If time exceeds 70 minutes in the first month, you may bill CPT 99494 in addition to 99492, once for each additional 30-minute block of care.
All time must be:
When to Use CPT 99484: Common Scenarios and Use Cases
CPT 99484 should be used when clinical staff, under the supervision of a physician or qualified healthcare professional, spend at least 20 minutes in a calendar month managing a patient’s behavioral health needs as part of an integrated care plan. These services must be non-face-to-face, and the code can be billed once per month per patient, regardless of how much time is spent beyond the 20-minute threshold.
Here are examples of how CPT 99484 is used in practice:
CPT 99492 Billing Requirements and Eligibility
CPT 99492 is used to report the first 70 minutes of Collaborative Care Model (CoCM) services in the initial month of psychiatric integration. This model requires a structured partnership between a behavioral health care manager, a psychiatric consultant, and the patient’s primary care provider or billing QHP.
To bill CPT 99492, the following conditions must be met:
Patient Eligibility Criteria
- The patient has one or more diagnosed behavioral health conditions, such as:
- Major depressive disorder (MDD)
- Generalized anxiety disorder (GAD)
- PTSD or trauma-related disorder
- Substance use disorder
- Other ICD-10 coded behavioral health diagnoses
- The condition is actively being treated and integrated into the primary care plan
Care Plan Requirements
- A structured behavioral health care plan must be:
- Developed or reviewed during the billing month
- Based on validated assessments (e.g., PHQ-9, GAD-7)
- Maintained and updated collaboratively by the BHCM, psychiatric consultant, and billing provider
- The plan should include:
- Behavioral health goals
- Planned interventions
- Clinical outcome measures
- Follow-up strategy and documentation of progress
Provider Requirements
- The billing provider must be a physician, NP, or PA overseeing the plan
- Clinical staff may perform the services, but they must operate under general supervision
- The billing provider must review staff documentation and ensure care plan continuity
Service and Time Requirements
- At least 36 minutes of CoCM activity must be completed in the first calendar month
- Activities must include:
- Behavioral health assessment and symptom tracking (e.g., PHQ-9)
- Patient engagement and follow-up
- Coordination with the psychiatric consultant and primary care team
- Treatment plan development and documentation
- Services must be:
- Non-face-to-face
- Performed by the CoCM team under general supervision
- Distinct from other care management time billed under CCM, PCM, or TCM codes
Billing Limitations
- CPT 99492 can be billed only once per patient, and only in the first month of CoCM services
- If CoCM services continue in subsequent months, use CPT 99493
- If time exceeds 70 minutes in the first month, add CPT 99494 for each additional 30-minute block
CPT 99492 Billing Documentation Checklist
To compliantly bill CPT 99492, the following must be clearly documented in the patient record:
- A behavioral health diagnosis supported by ICD-10 coding
- Examples include MDD, GAD, PTSD, or substance use disorder
- Diagnosis must be active and the focus of care during the billing month
- A behavioral health care plan that was:
- Developed or updated during the billing period
- Based on a validated screening tool (e.g., PHQ-9, GAD-7)
- Integrated into the patient’s overall care plan
- Documented with:
- Behavioral goals
- Planned interventions
- Outcome tracking and follow-up strategy
- A clearly defined CoCM team, including:
- Billing provider (physician, NP, or PA)
- Behavioral health care manager (BHCM)
- Psychiatric consultant (e.g., psychiatrist or clinical psychologist)
- A minimum of 36 minutes of CoCM services delivered in the calendar month
- Services must be:
- Non-face-to-face
- Performed by the CoCM team
- Directed by the billing provider
- Logged with start/stop or cumulative time totals
- Activities may include:
- Reviewing structured assessments (e.g., PHQ-9)
- Tracking symptoms
- BHCM follow-up with the patient
- Team consultation and treatment adjustments
- Services must be:
- Psychiatric consultant review and treatment recommendations
- Must be documented in the chart or via care team communication
- Consultant does not see the patient directly, but provides clinical oversight
- An attestation or documentation note from the billing provider, confirming:
- Review of BHCM activities and documentation
- Coordination with the psychiatric consultant
- Oversight of the full CoCM process
Common CPT 99492 Billing Mistakes (and How to Avoid Them)
❌ Billing 99492 Without a Psychiatric Consultant
CPT 99492 requires documented involvement of a psychiatric consultant, such as a psychiatrist or clinical psychologist. If no consultant is involved in diagnosis or treatment planning, the service does not meet CoCM criteria.
❌ Using 99492 for Staff-Only Behavioral Health Services
This code is not for stand-alone clinical staff time. A behavioral health care manager, billing provider, and psychiatric consultant must all be documented as part of the collaborative team.
❌ Billing for Fewer Than 36 Minutes
You must document at least 36 minutes of CoCM services in the first month. If time falls short, the code is not billable—even if a care plan is created.
❌ Billing 99492 More Than Once Per Patient
CPT 99492 is a first-month only code. It may be billed only once per patient. For subsequent months, use CPT 99493, with 99494 for additional time blocks.
❌ Double Billing With Other Care Management Codes
❌ Insufficient Documentation of Care Team Activity
You must record:
- The behavioral health diagnosis and validated screening results
- All time logs across the team, including BHCM, consultant, and provider coordination
- Psychiatric consultant input and care plan recommendations
- Oversight by the billing provider and plan review documentation



